Summary points
Most patients with pyogenic abscesses will require percutaneous drainage and antibiotics. A cause can be identified in 85% of cases of liver abscess, most commonly gall stones, diverticulitis, or appendicitis. Amoebic abscesses are commonest, can be treated by metronidazole alone in 95% of cases. Liver abscesses are caused by bacterial, parasitic or fungal infection. Pyogenic abscesses account for 3/4 of hepatic abscess in developed countries. Amoebic abscesses are more common, and, worldwide, amoebae are the commonest cause.

Pyogenic liver abscesses
Aetiology
-secondary to infection originating in the abdomen.
-Cholangitis due to stones or strictures is the commonest cause
-abdominal infection due to diverticulitis or appendicitis.
-In 15% of cases no cause (cryptogenic abscesses).
-Diabetes mellitus has been noted in 15% of adults with liver abscesses.
Microbiology

-polymicrobial infection usually with Gram negative aerobic and anaerobic organisms
-Bowel origin (most common)
Escherichia coli, Klebsiella pneumoniae, bacteroides, enterococci, anaerobic streptococci, and microaerophilic streptococci
-Primary infection is bacterial endocarditis or dental sepsis
Staphylococci, haemolytic streptococci and Streptococcus milleri
-Immunosuppression (AIDS), intensive chemotherapy, and transplantation
fungal or opportunistic organisms
Clinical features
Classic presentation
-abdominal pain
-swinging fever
-nocturnal sweating,
-vomiting
-anorexia
-malaise, and
-weight loss
-Insidious onset in elderly people and patients may present with a primary infection (such as diverticulitis or appendicitis) before developing symptoms from their liver abscess.
-Single abscesses-gradual in onset and are often cryptogenic.
-Multiple abscesses are associated with more acute systemic features
Clinically
-Liver is enlarged and tender
-percussion over the lower ribs aggravates the pain
-Jaundice occurs only in the late stage
-Right upper quadrant pain or hepatomegaly
-Fever of unknown origin.
Investigations
-Leucocytosis - two thirds of patients
-Anaemia of chronic infection
-Raised ESR
-Alkaline phosphatase raised
-Hypoalbuminaemia
-serum transaminase may be marginally abnormal.
-Plain abdominal X-ray
-hepatomegaly
-air fluid level in abscess cavity
-right diaphragm raised
-pleural reaction or pneumonic consolidation
-Ultrasonography
-initial method of imaging
-used to guide aspiration
 -CT Scan is useful to identify other intra-abdominal abscesses.
-CT Scan is useful to identify other intra-abdominal abscesses.
-ERCP is used to define the site and cause of biliary obstruction and to allow biliary stenting and drainage.
Treatment
-Empirical broad spectrum IV antibiotic tx should be started as soon as an abscess is diagnosed
-penicillin, aminoglycoside and metronidazole against E coli, K pneumoniae, bacteroides, enterococcus, and anaerobic streptococci
-In elderly with impaired renal fx a 3rd generation cephalosporin should be used instead of an aminoglycoside. The regimen should be modified after culture has identified. Treatment is continued for two to four weeks depending on the number of abscesses, the clinical response, and the potential toxicity of the chosen regimen.
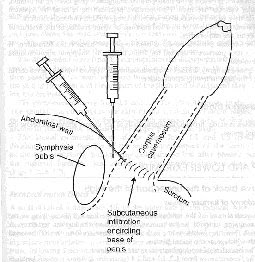
-Antibiotics alone are effective in only a few patients, and most patients will require percutaneous aspiration or catheter drainage guided by ultrasonography or CT scan. Underlying cause should be treated.
-Early diagnosis, tx with appropriate antibiotics, and selective drainage can reduced mortality.
-Factors that increase risk of death include shock, ARDS, DIVC, immunodeficiency states, severe hypoalbuminaemia, diabetes, ineffective surgical drainage, and associated malignancy.
Amoebic liver abscess

Introduction
About 10% of the world's population is chronically infected with Entamoeba histolytica. Third commonest parasitic cause of death. Occurs most commonly in tropical and subtropical climates. Overcrowding and poor sanitation are the main predisposing factors.
Pathogenesis
The parasite is transmitted through the faeco-oral route with the ingestion of viable protozoal cysts. The cyst wall disintegrates in the small intestine, releasing motile trophozoites. These migrate to the large bowel, where pathogenic strains may cause invasive disease. Mucosal invasion results in the formation of flask-shaped ulcers through which amoebae gain access to the portal venous system. The abscess is usually solitary and affects the right lobe in 80% of cases. The abscess contains sterile pus and reddish-brown ("anchovy paste") liquefied necrotic liver tissue. Amoebae are occasionally present at the periphery of the abscess.
Clinical presentation and diagnosis
 Symptoms from a few days to several weeks before presentation. Pain is a prominent feature, toxic, febrile and chronically ill. The patient is usually resident in endemic area, although there may be no history of diarrhoea. Leucocytosis with 70-80% polymorphs (eosinophilia is not a feature), raised ESR, and moderate anaemia. Severe disease and multiple abscesses- alkaline phosphatase and bilirubin are raised. Stools contain cysts, or in the case of dysentery, haematophagous trophozoites. Chest radiography - raised right hemidiaphragm with atelectasis or pleural effusion. Ultrasonography - size and position of the abscess and is useful when aspiration is necessary and to assess response to treatment. Indirect haemagglutination titres for entamoeba are raised in over 90% of patients. Complications occur as a result of secondary infection or rupture into adjacent structures such as pleural, pericardial, or peritoneal spaces. 2/3 of ruptures occur intraperitoneally and 1/3 intrathoracically.
Symptoms from a few days to several weeks before presentation. Pain is a prominent feature, toxic, febrile and chronically ill. The patient is usually resident in endemic area, although there may be no history of diarrhoea. Leucocytosis with 70-80% polymorphs (eosinophilia is not a feature), raised ESR, and moderate anaemia. Severe disease and multiple abscesses- alkaline phosphatase and bilirubin are raised. Stools contain cysts, or in the case of dysentery, haematophagous trophozoites. Chest radiography - raised right hemidiaphragm with atelectasis or pleural effusion. Ultrasonography - size and position of the abscess and is useful when aspiration is necessary and to assess response to treatment. Indirect haemagglutination titres for entamoeba are raised in over 90% of patients. Complications occur as a result of secondary infection or rupture into adjacent structures such as pleural, pericardial, or peritoneal spaces. 2/3 of ruptures occur intraperitoneally and 1/3 intrathoracically.
Treatment
-95% of uncomplicated amoebic abscesses resolve with metronidazole alone (800 mg tds for 5 days).
-Adequate nutrition and pain relief are important. Clinical symptoms usually improve greatly within 24 hours.
-Lower doses of metronidazole are often effective in invasive disease but may fail to eliminate the intraluminal infection, allowing clinical relapses to occur.
-After the amoebic abscess has been treated, patients are prescribed diloxanide furoate 500 mg 8 hourly for 7 days, to eliminate intestinal amoebae.
-U/S guided needle aspiration - serology negative results, abscess is large > 10 cm, not respond to tx or impending peritoneal, pleural, or pericardial rupture.
-Surgical drainage - ruptured causing amoebic peritonitis or not responded to drugs despite aspiration or catheter drainage.