INTUBATION
1) Anatomy, nerve innervation,phatologic cond. & method of assessment.
2) Physiologic consequences & complication.
3) Anticipate pt. with difficult airway.
4) Formulate & implement alternative plan in various clinical situation.

 History
HistorySn/Sm suggest abnormal airway
•SOB
•Hoarsenes ( rheumatoid artritis- criocotenoid cartilage – narrowing Lx opening.)
Previous surgery, trauma, neoplasia of airway
2) protruding teeth(edentulous)- disturb seal mask, loose, capped, prosthetic teeth.
3) Cleft, high-arch palate
4) Large big tongue( trisomy 21, mucopolysaccharidoses, beckwith-weidemann syndrom)
•Mallampati classification
•Temporomandibular joint mobility
( ankylosis,long term type1 DM, pain due to trauma)
•Distance lower border mandible to thyroid notch > 6.5 cm (adult)


 INDICATIONS OF INTUBATION
INDICATIONS OF INTUBATION1) Inabiliy to oxygenate patient (SpO2 <>
2) Inability to ventilate patient (rising PaCO2, respiratory acidosis, mental status change or other symptoms)
3) Patient unable to protect the airway.
1) Neck immobility or increased risk of neck trauma (e.g. rheumatoid arthritis, cervical spine injury, etc.)-consider fiberoptic intubation.
2) Inability to open mouth (e.g. trismus, scleroderma, surgical wiring, etc.)- consider nasal intubation, either blind or fiberoptic, or surgical airway.
2) Airways
3) Laryngoscopes
4) Endotracheal tubes + stylet.
•Adult male: 7.0,7.5,8.0
•Adult female: 6.5,7.0,7.5
•Children > 1 year age
size= (age(yr) +16 )/ 4
5) Length of tube cm= 12 + (age/2)
6) Suction.

- Assemble equipment
- Calculate doses and draw medications into syringes
- Check IV access and flush fluid
- Preparation And Equipment (Always Have Suction Available)
- Head Position - Alignment Of Oral, Pharyngeal, and Laryngeal Axes ,(sniffing position)
- Choice Of Laryngoscope And Endotracheal Tube
dose- 0.3 mg/kg
advantage-Good for low blood pressure; okay in hypovolemia
cautions- Nausea and vomiting on emergence
dose- 1.5 mg/kg
advantage- Good for low blood pressure, hypovolemia; good in asthma
Caution in elevated intracranial pressure or heart disease
dose- 2 - 2.5 mg/kg
advantage- Rapid onset and recovery
Caution if hypovolemic or risk of hypotension
dose- 3 - 5 mg/kg
advantage- Multiple drug interactions
dose 1 - 1.5 mg/kg
characteristic- Rapid onset, rapid recovery; fasciculation
Contraindicated in hyperkalemia, crush injury, renal failure, extensive burns, elevated intracranial or intraocular pressure
dose 0.6- 1.2 mg/kg
characteristic- No fasciculation
cautions- Longer acting-may be problematic if intubation attempt fails
dose 0.08 - 0.1 mg/kg
dose 0.4 - 0.5 mg/kg
- Sniffing Position
- Laryngoscope In LEFT Hand
- Open Mouth


Laryngoscopic view may be clasified into four grades:
 Grade I = visualization of the entire laryngeal aperture.
Grade I = visualization of the entire laryngeal aperture. Grade II = visualization of just the posterior portion of the laryngeal aperture.
Grade II = visualization of just the posterior portion of the laryngeal aperture. Grade III = visualization of only the epiglottis.
Grade III = visualization of only the epiglottis. Grade IV = visualization of just the soft palate only, not even the epiglottis is visible.
Grade IV = visualization of just the soft palate only, not even the epiglottis is visible.Laryngoscopic View Grades
Grade II or III laryngoscopic views are relatively common and occur in 1 to 18% of surgical patients. The Grade III view occurs in about 1-4% of patients. A severe grade III or grade IV view with failed endotracheal intubation occurs 0.05 of 0.35% of patients.
It may be helpful to the next anesthesiologist to record both the grade of laryngoscopic view achieved, the patient position and the technique.
Laryngoscopic View Grades
 Alternatives To Orotracheal Intubation Under Anesthesia
Alternatives To Orotracheal Intubation Under AnesthesiaAwake Orotracheal Intubation
Nasotracheal Intubation - Awake Blind Nasal - Nasotracheal Intubation After Induction
Intubation With Fiberoptic Bronchoscope
- Awake versus Under Anesthesia
- Orotracheal versus Nasotracheal
Retrograde Intubation
Verification Of Correct Tube Placement
- The most reliable method for determination of tube placement is direct vision of the endotracheal tube passed through the vocal cords
- Symmetric Chest Movement
- Symmetric Breath Sounds
- End tidal Carbon Dioxide - Greater Than 30 For 3-5 Breaths
- Condensation Of Water In The tube
- Palpation Of Cuff In Suprasternal Notch
- Fiberoptic Bronchoscopy

RAPID SEQUENCE INDUCTION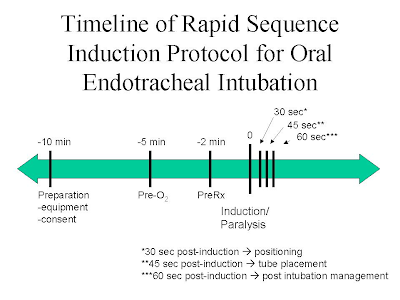 Sequence and rapid method of securing airway, to minimizes aspiration in process of intubation
Sequence and rapid method of securing airway, to minimizes aspiration in process of intubation
•Pt preoxygenated for 5 minutes / 4 max deep breath within 30 scd/ 3 vital capacity breath 100% O2.
•No assisted breathing until airway isolated
•Nondepolarizing MR - scolin
•Applied cricoid pressure (sellick’s maneuver)
*All process should be completed in 60 sc post induction
Complication of endotracheal intubation
During intubation
•Laryngospasm
•Laceration,bruising lips,tongue,pharynx
•#,chipping,dislogement of teeth
•Perforation trachea,esophagus
•Retropharyngeal dissection
•# or dislocation cervical spine
•Trauma to eyes
•Haemorrage
•Bactremia
•Aspiration gastric content/ FB
-Endobrachial or esophageal intubation
-Dislocation arytenoid cartilages or mandible
-Hypoxemia, hypercarbia.
-Bradycardia, tachycardia
-Hypertension
-Increased intracranial or intraocular pressure
Complication with tube insitu
-Accidental extubation
-Endobrachial intubation
-Obstruction / kinking
-Bronchospasm
-Ignation of tube by laser device
-Aspiration
-Sinusitis
-Excoriation of nose or mouth
Complication after extubation
-Laryngospasm
-Aspiration –gastric content, blood, FB
-Glottic,subglottic, uvular edema
-Dysphonia,aphonia
-Paralysis of vocal cord, hypoglossal,lingual nerves
-Sore throat
-Noncardiogenic pulmonary edema
-Laryngeal incompetance.
-Soreness, dislocation jaw
-Tracheomalacia
-Glottic,subglottic or tracheal stenosis
-Vocal cord granulomata.





